Airway Dentistry in Dubai: Snoring, Sleep-Disordered Breathing & TMJ-BDS Care (Children & Adults)
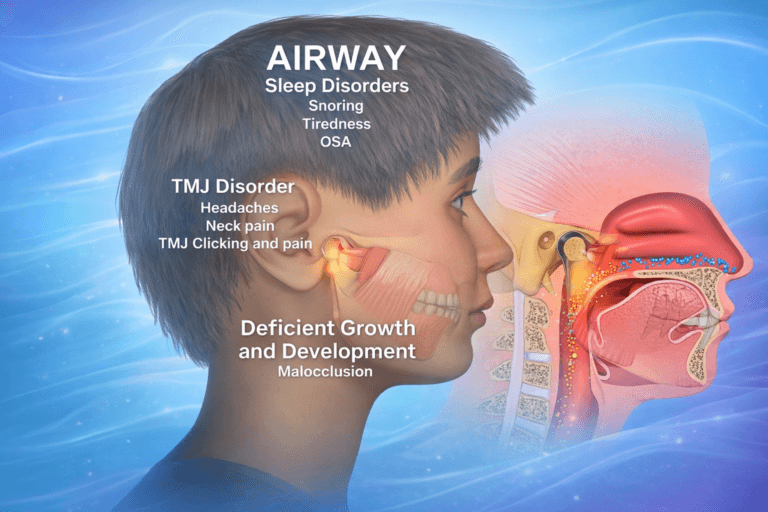
Why Airway Health Matters
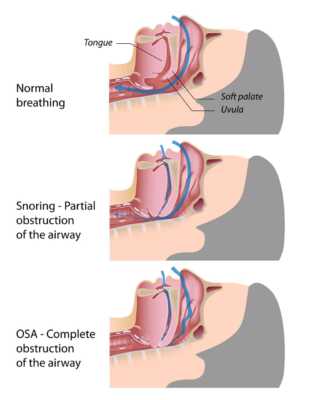
Snoring can be a sign of increased airway resistance. While it may be benign, persistent loud snoring, especially when accompanied by daytime sleepiness, morning headaches, or witnessed breathing pauses, warrants a medical evaluation for sleep-disordered breathing.
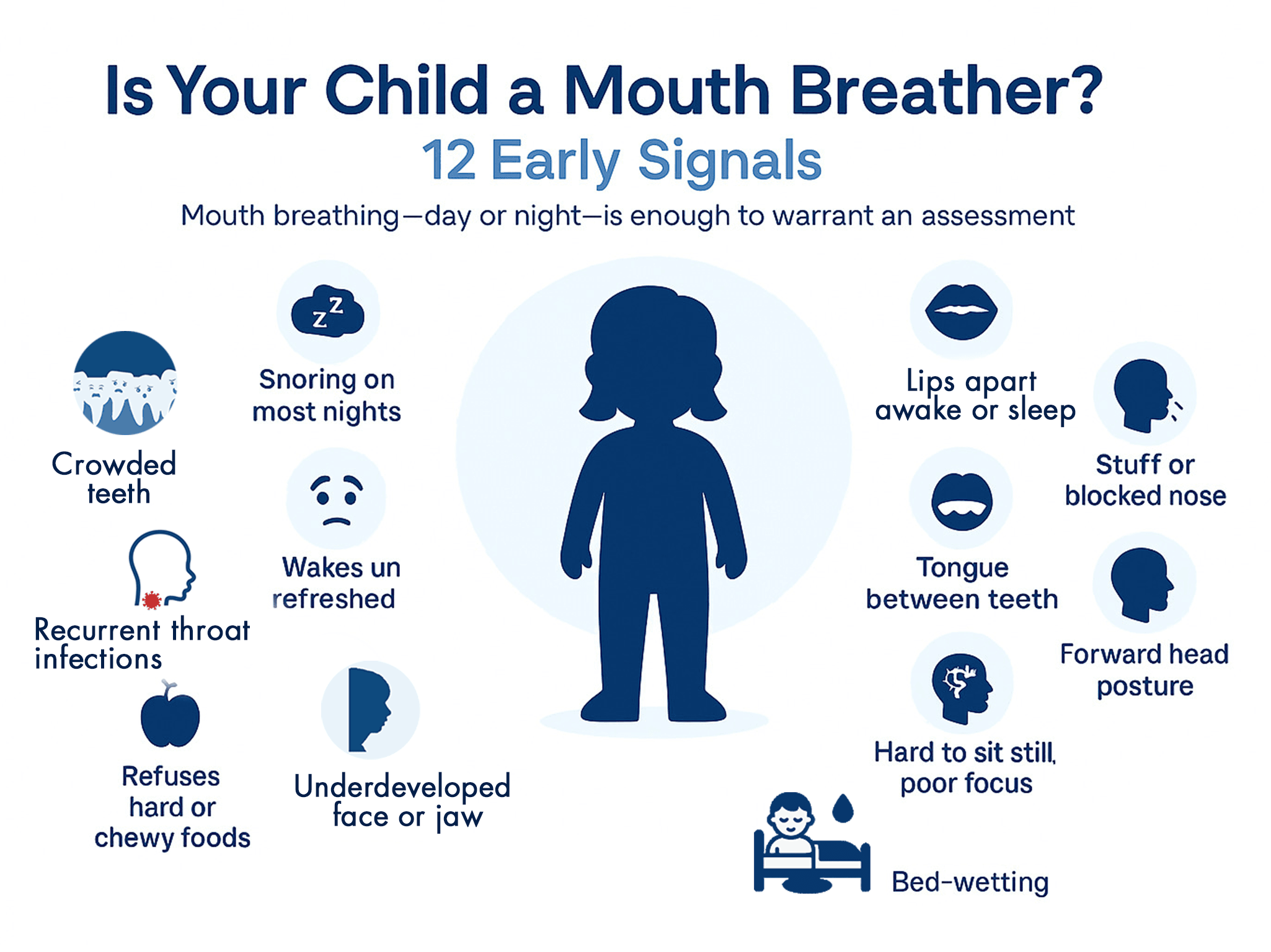
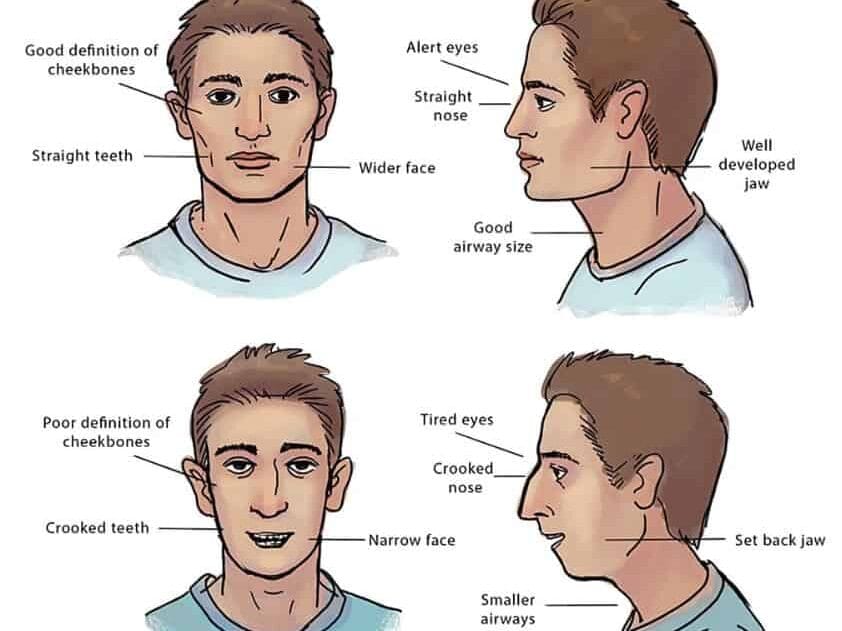
Sleep-disordered breathing can affect both children and adults. In children, factors such as chronic nasal obstruction, habitual mouth-breathing, low tongue posture, and narrow arches may contribute to noisy breathing and disturbed sleep. Recent medical literature increasingly recognizes chronic mouth breathing in children as more than a habit, as it may be associated with changes in craniofacial development and overall health, including learning and attention difficulties and hyperactive-like behavior.
In adults, airway restriction may contribute to chronic fatigue, lack of concentration, sleep apnea frequent headaches, and cardiovascular health risks. It also may overlap with jaw-position factors, soft-tissue collapse, and parafunction (sleep bruxism) that can contribute to TMJ-BDS symptoms.
Common Signs We Screen For
Children
• Habitual open-mouth posture or mouth-breathing
• Snoring or noisy breathing most nights
• Restless sleep, frequent waking, or unusual sleep positions
• Breathing pauses, gasping, or heavy breathing during sleep
• Bed-wetting, morning dry mouth, or waking unrefreshed
• Daytime tiredness, irritability, or difficulty focusing
• Dark under-eye circles, narrow arches, or dental crowding
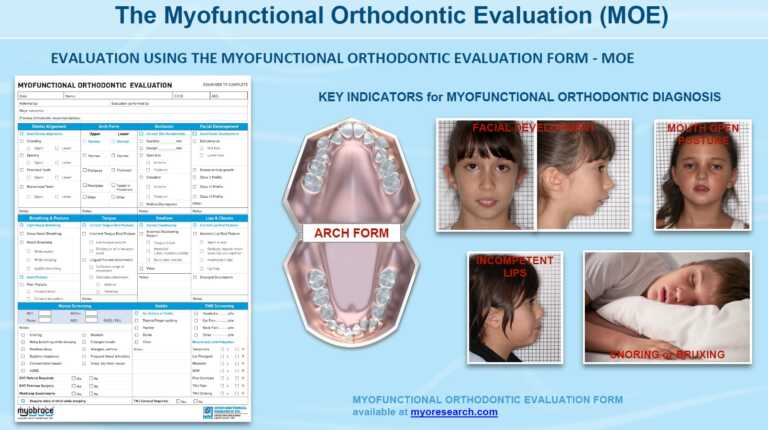
Our Approach at Vilafortuny
Ready to Get Started?
If you or your child has persistent mouth breathing, snoring, difficulties in concentration, restless sleep, daytime fatigue, or jaw/TMJ symptoms, book an airway consultation. We will screen risk factors, coordinate medical evaluation when indicated, and discuss appropriate dental support options.
Frequently Asked Questions
What is the first step at your clinic?
We begin with an airway-informed dental consultation: sleep and symptom history, risk screening, functional breathing review, and an oral/jaw assessment. If findings suggest risk of sleep-disordered breathing, we recommend medical evaluation and, when appropriate, a sleep study.
Do I need a sleep study?
Not always. If severe sleep-disordered breathing is suspected, a sleep study (at home or in a sleep lab) will be recommended. Sleep Study is the standard way to confirm diagnosis and severity. For primary snoring without red-flag symptoms, our team may decide a sleep study is not required.
How do oral appliances for snoring/sleep-disordered breathing work?
In suitable children and adults, an oral appliance is worn overnight during sleep, and in some cases for a short period during the day as part of a myofunctional program. Depending on the clinical indication, this may be a myofunctional appliance or a custom mandibular advancement device that gently positions the lower jaw and tongue forward to help reduce airway collapse and support nasal breathing. Your dentist monitors fit and comfort and, when a mandibular advancement device is used, adjusts (titrates) it for effectiveness in coordination with your sleep expert.
How is a myofunctional appliance different from a mandibular advancement device?
A myofunctional appliance is used as part of a program that targets oral posture and function (lip seal, tongue posture, and nasal breathing support). Mandibular advancement devices primarily reposition the jaw forward during sleep. The best option depends on age, anatomy, symptoms, and medical diagnosis.
Is snoring treatment permanent?
It depends on the cause. Appliances generally manage symptoms while worn. Functional rehabilitation and, in some cases, structural interventions may support longer-term stability, but no single option can be guaranteed for every patient. Our medical team will create an individual treatment plan, and will discuss it with you after the assessment.
Do you treat children who mouth-breathe or snore?
Yes. We assess oral and functional contributors and coordinate referral to a pediatrician/ENT or sleep expert when needed. Treatment planning is age-appropriate and focused on healthy breathing, sleep quality, craniofacial development, and overall wellbeing.
Can airway dentistry help with clenching, bruxism, or TMJ-BDS symptoms?
It can. Many adults with sleep-disordered breathing also clench or grind. We evaluate airway-related and jaw-function contributors and may provide TMJ-BDS-oriented appliance support and functional rehabilitation, while coordinating medical evaluation when indicated.
What role does CBCT imaging play?
CBCT can support assessment of craniofacial anatomy and airway-adjacent structures when clinically justified. It supports treatment planning, but it does not diagnose sleep-disordered breathing; diagnosis relies on a physician-interpreted sleep study.
Is CPAP the only effective option?
CPAP is highly effective for many patients. For some adults with primary snoring or mild to moderate sleep-disordered breathing who cannot tolerate CPAP or prefer an alternative, oral appliance therapy can be an evidence-supported option under medical guidance.
How is a dentist going to fix behavior?
A dentist doesn’t “treat behavior” directly – but we often discover breathing and sleep problems that can affect a child’s mood, focus, and energy. If a child can’t breathe well through the nose, their only option is mouth breathing. Over time, this can change jaw and palate growth, crowd the airway, and contribute to poor-quality sleep. Poor sleep and reduced airflow at night can show up as hyperactivity, irritability, and poor concentration during the day due to low oxygen level caused by mouth breathing. We look for early signs in the mouth and face, assess breathing and myofunctional patterns, and provide appropriate dental support and referrals to ENT/sleep experts when needed – with the goal of helping the child breathe better, sleep better, and function better.
Does every daytime sleepy child need a sleep screening?
Not necessarily. Daytime sleepiness can be caused by common issues like too little sleep, an irregular bedtime routine, or a temporary illness. But if daytime sleepiness is frequent or persistent-especially when paired with signs of sleep-disordered breathing (SDB) (snoring most nights, mouth breathing, restless sleep, pauses/gasping, bedwetting, morning headaches, or attention/behavior concerns), then a sleep screening is recommended. In our clinic, we can screen and assess airway and myofunctional factors and, when indicated, coordinate with your child’s pediatrician, ENT, or a sleep expert for further evaluation (which may include validated questionnaires and, in some cases, a sleep study).